”The 3D model provided a more accurate diagnosis, increased our confidence in determining that the tumour was unresectable, allowed us to address the right hepatic artery first, and helped us avoid manoeuvres that could have been irreversible
Dr. José Mir LabradorHead of Section, Hepatopancreatobiliary Surgery, Hospital General Universitario de Valencia
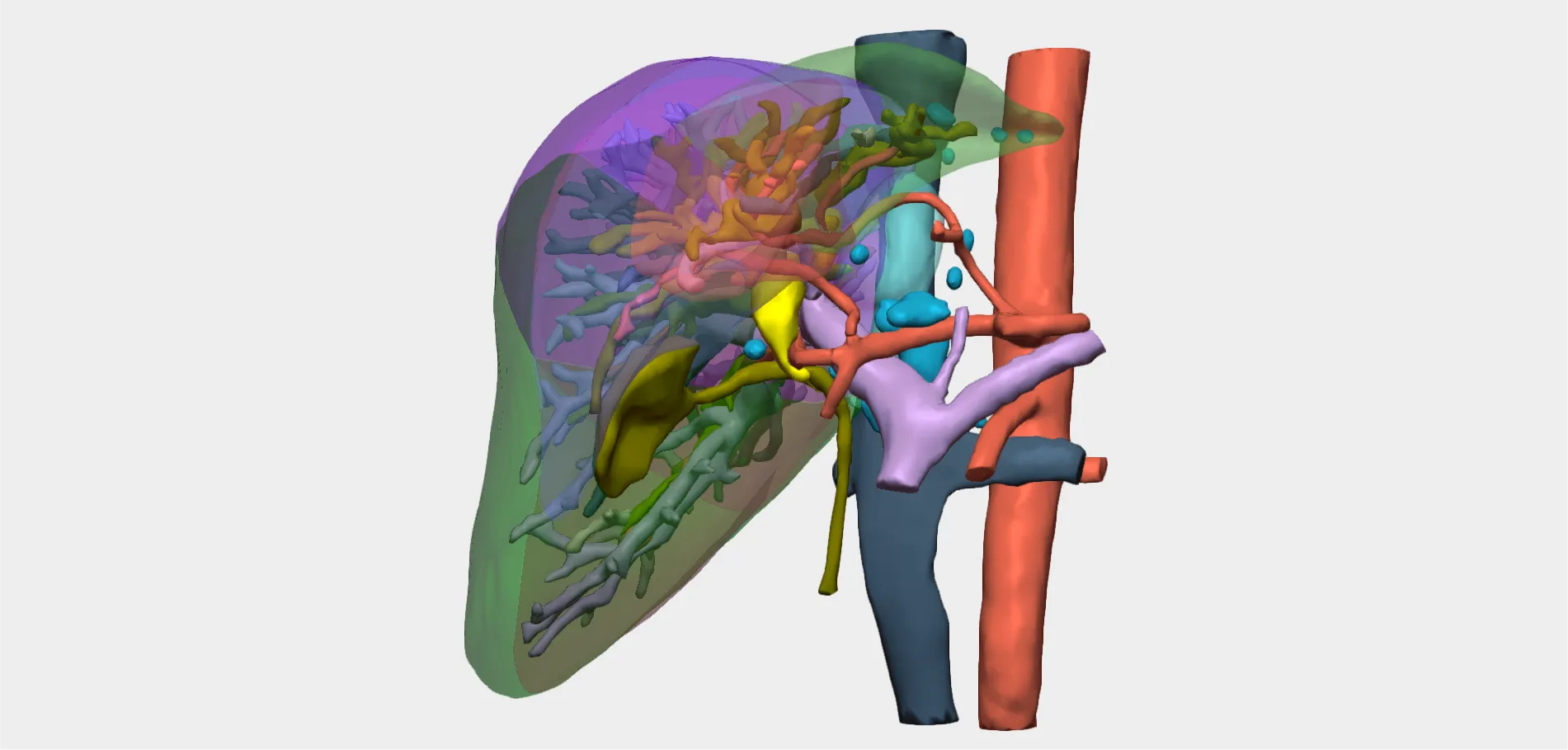
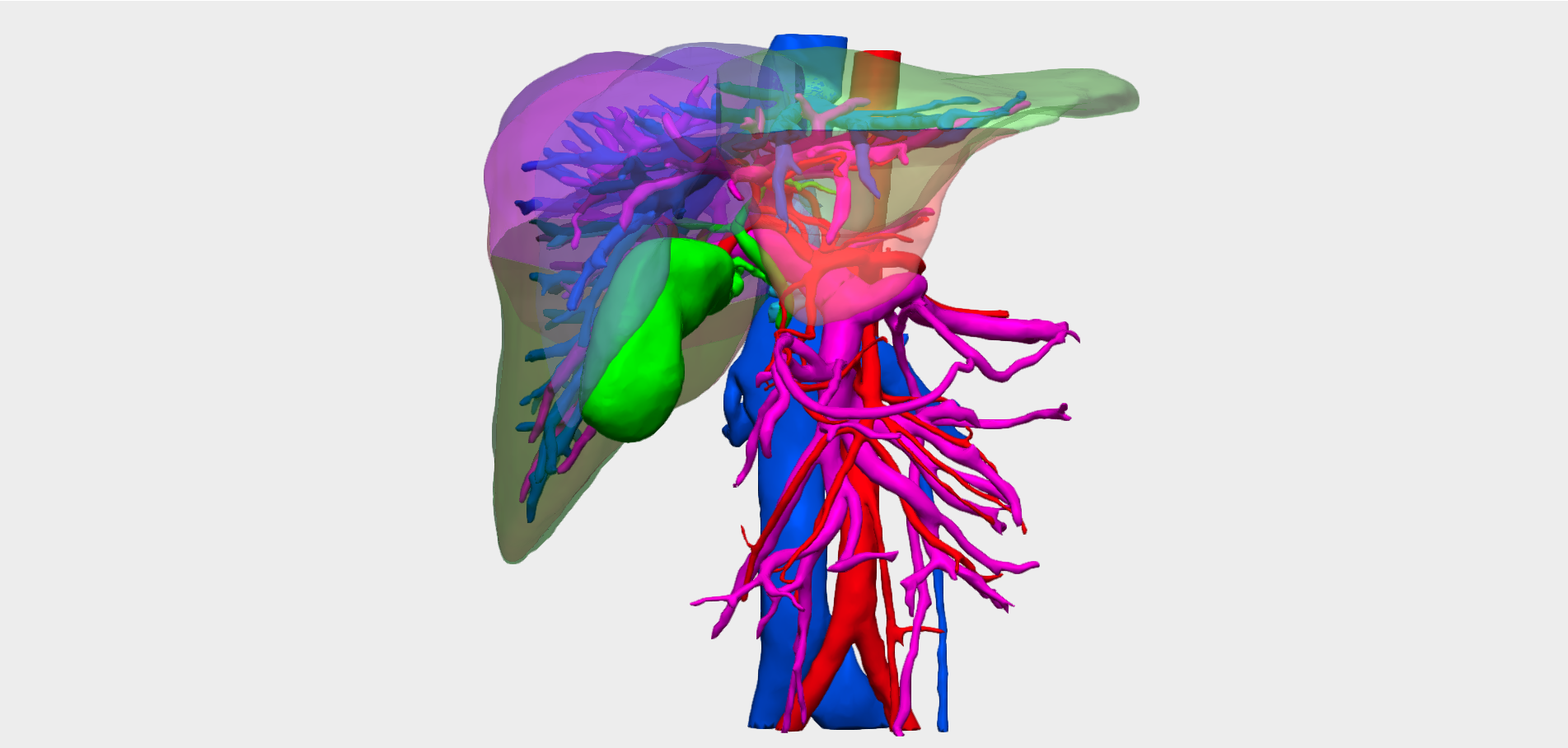
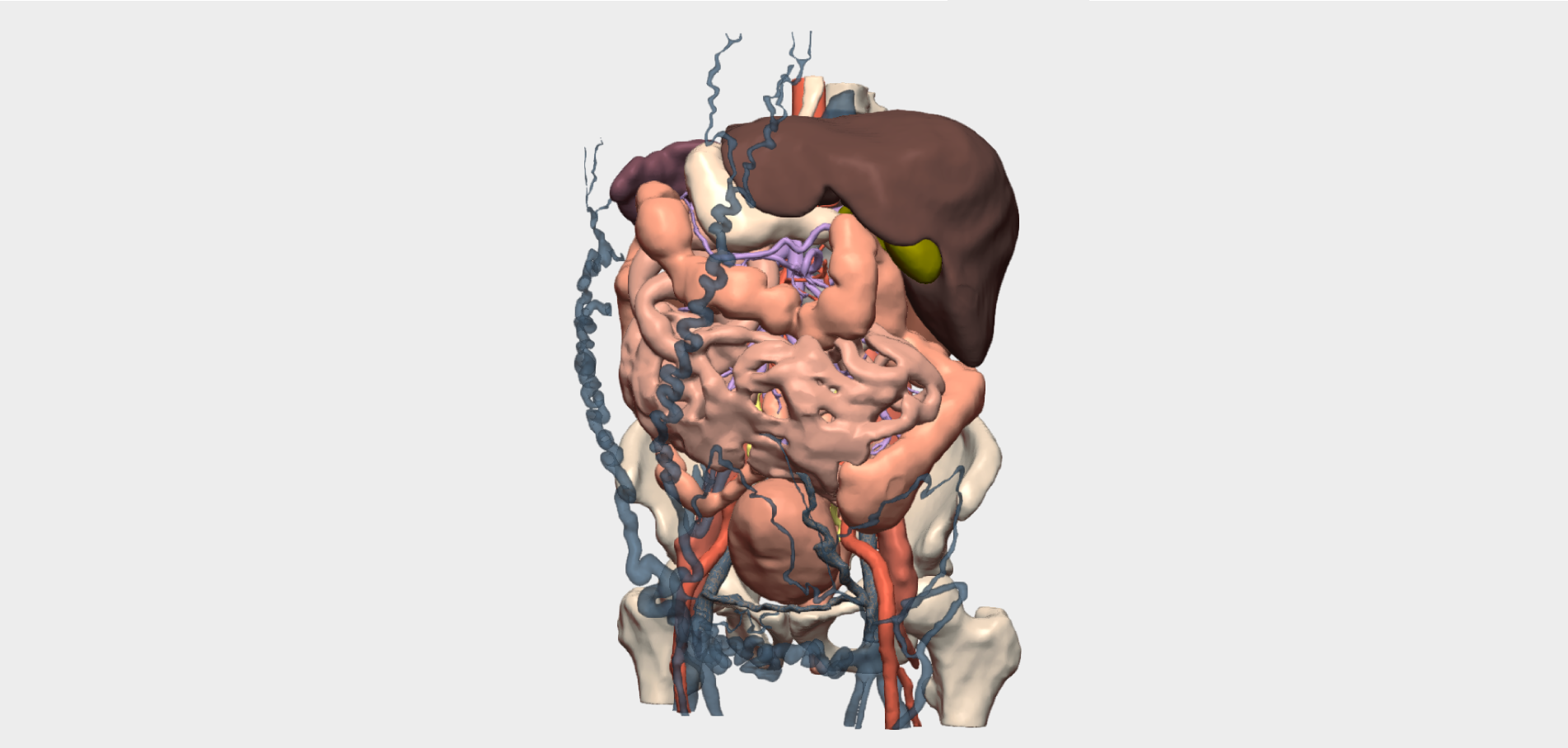
In highly complex perihilar cholangiocarcinoma, such as Klatskin tumours, 3D-assisted surgical planning is becoming increasingly relevant. Patient-specific 3D models enable accurate reconstruction of individual anatomy, facilitating detailed assessment of tumour extent, its relationship with vascular structures and adjacent organs, and, ultimately, safer and more personalised surgical decision-making.Below, we present a clinical case in which a 3D model was decisive in avoiding unnecessary surgery, allowing the team to select the most appropriate therapeutic strategy for a cancer of exceptional complexity.
Clinical Case Presentation
A 71-year-old female patient presented with obstructive jaundice. Magnetic resonance imaging (MRI) revealed a Klatskin tumour type IIIb–IV, infiltrating the left portal vein branch and appearing to be in contact with the right hepatic artery. Relevant medical history included arterial hypertension, diabetes mellitus, pernicious anaemia, hypothyroidism, asthma and a previous ischaemic stroke.
Initial Assessment with Conventional Imaging
MRI findings suggested tumour contact with the right hepatic artery; however, the feasibility of resection and the exact degree of vascular involvement could not be clearly determined. An exploratory robotic approach was initially proposed, with possible left hepatectomy, lymphadenectomy, caudate lobe resection and potential resection and reconstruction of the right hepatic artery.
Contribution of 3D Reconstruction to Redefining Surgical Strategy in Klatskin Tumour
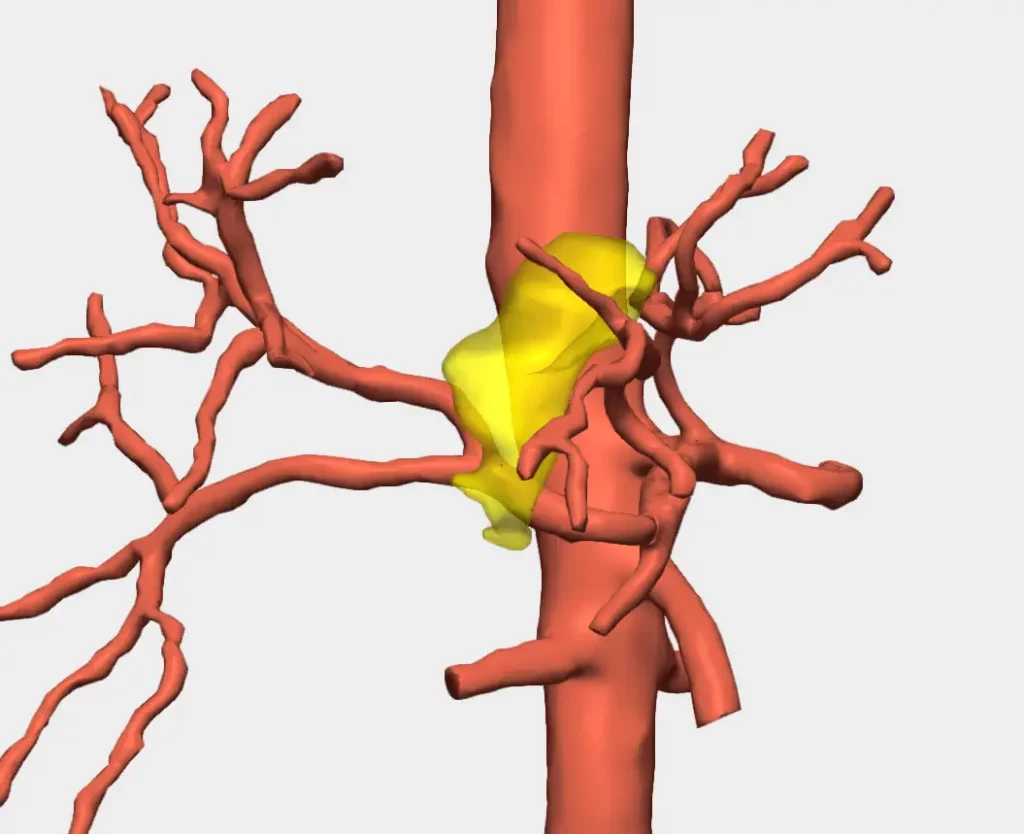
The creation of a patient-specific 3D model enabled precise anatomical visualisation, allowing accurate evaluation of the tumour’s relationship with the right hepatic artery. This reconstruction demonstrated that the tumour involved the artery at the level of bifurcation between the anterior and posterior sectoral branches, thereby reclassifying the lesion as a Klatskin type IV tumour, which is considered unresectable.
Despite these findings, surgical exploration was undertaken to directly assess right-sided vascular involvement. Intraoperatively, dissection of the right hepatic artery proved impossible due to tumour infiltration, confirming the preoperative 3D assessment.
Conclusions and Clinical Benefits of 3D Models
“The 3D model provided a more accurate diagnosis, increased the likelihood of classifying the tumour as unresectable, allowed us to prioritise evaluation of the right hepatic artery, and prevented manoeuvres that could have resulted in irreversible damage,” explains Dr José Mir Labrador, Head of Section of Hepatobiliopancreatic Surgery at Hospital General Universitario de Valencia.
In addition to improving clinical decision-making, the information provided by the 3D reconstruction optimised operating theatre scheduling, allowing the available surgical time to be allocated to another patient on the waiting list.
In complex tumours such as extrahepatic cholangiocarcinoma, 3D models have become an essential tool for precise and efficient surgical planning. Their implementation not only supports preoperative diagnosis, but also increases the likelihood of optimal outcomes by tailoring the surgical approach to the patient’s true anatomical reality.

© 2026 Cella Medical Solutions