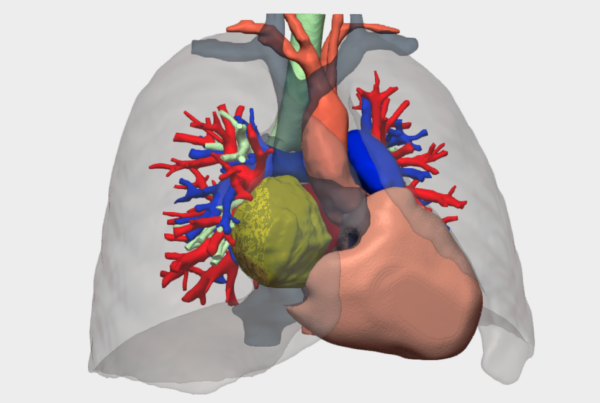
”The 3D reconstruction model enabled a much clearer mental understanding of the tumour anatomy and its relationship with the bronchovascular structures.
Dr. Carlos Gálvez MuñozThoracic Surgeon, Hospital General Universitario de Alicante
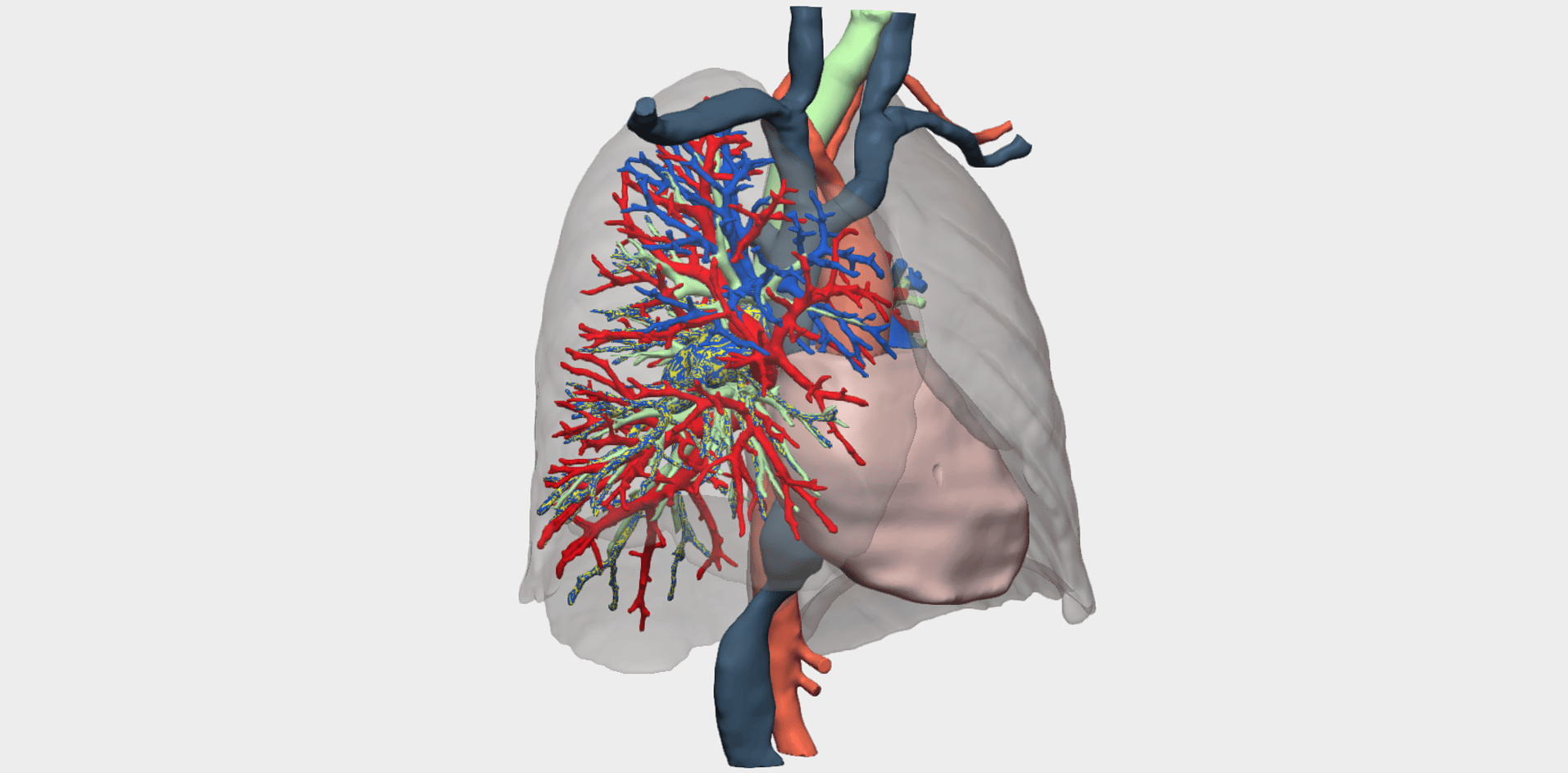
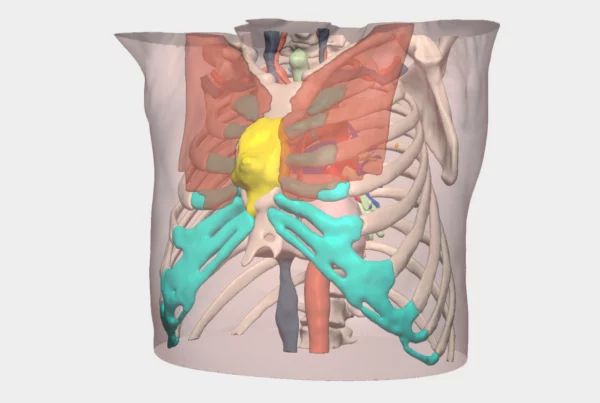
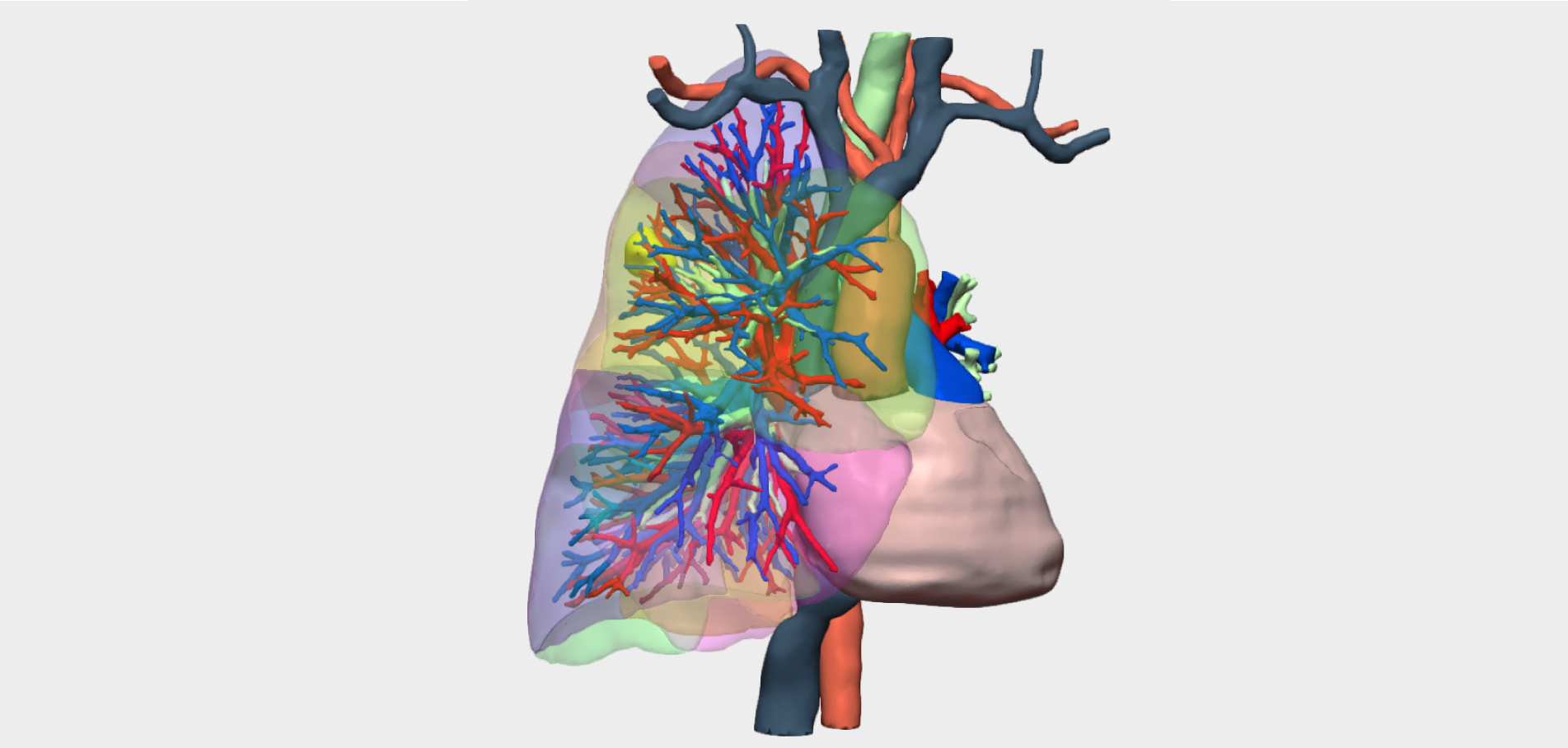
Pulmonary artery sarcoma is a rare malignancy with a complex diagnostic pathway, characterised by insidious growth and frequent misdiagnosis as conditions such as pulmonary thromboembolism. Three-dimensional reconstruction in this pathology represents an innovative tool for detailed assessment of tumour extent and its relationship with vascular and bronchial structures, facilitating surgical planning and improving overall disease understanding.
Clinical Case: Pulmonary Artery Sarcoma

We present the case of a 63-year-old female patient, a former smoker with an active lifestyle, who attended consultation due to progressive dyspnoea and chest pain. CT pulmonary angiography revealed findings compatible with pulmonary embolism at the level of the right interlobar pulmonary artery near the major fissure, and anticoagulation with low-molecular-weight heparin was initiated. Despite appropriate anticoagulation therapy and a venous Doppler ultrasound negative for deep vein thrombosis, a follow-up CT angiography was requested. This demonstrated a lesion in the right pulmonary artery with proximal progression towards the right upper lobe, raising suspicion of malignancy, most consistent with pulmonary artery sarcoma.
Subsequent investigations confirmed the following:
-
-
PET-CT: Hypermetabolic uptake (SUVmax CGM1) with no evidence of metastatic disease
-
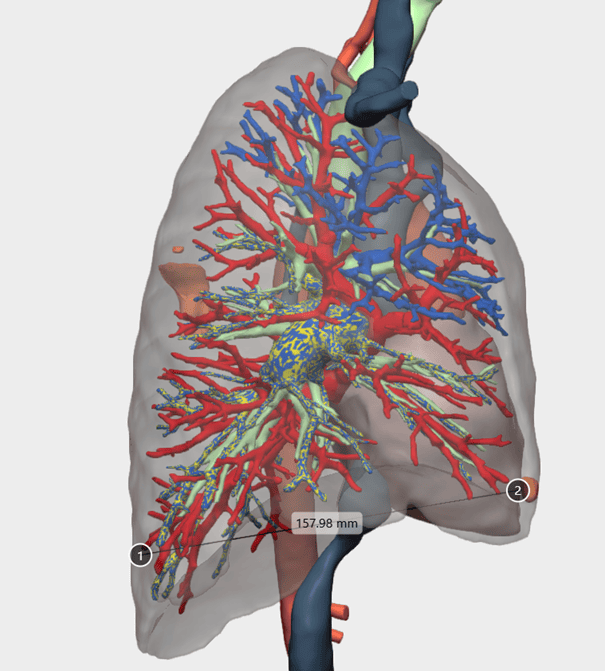
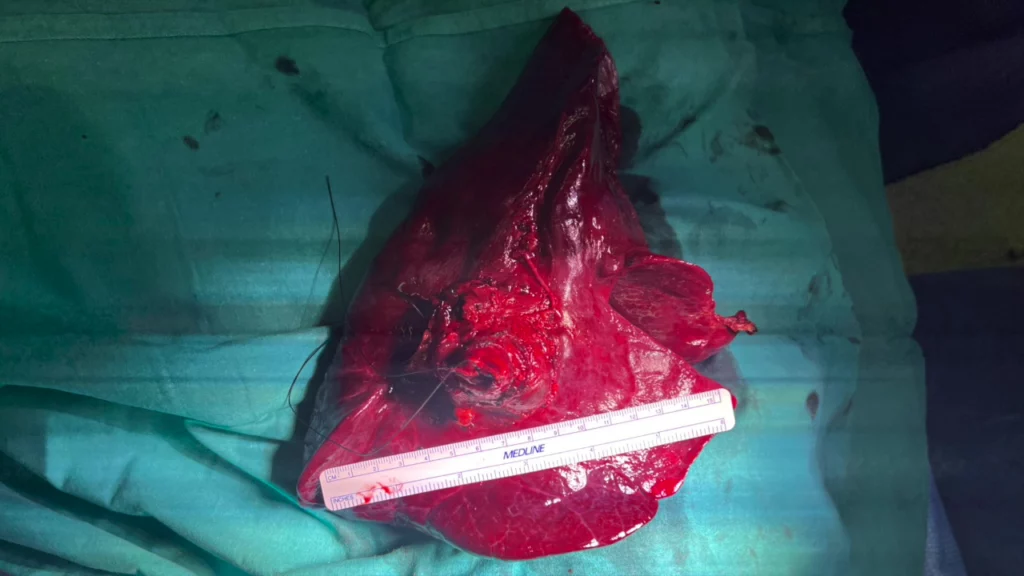
Thoracic MRI: A 5.9 × 3.2 × 3.4 cm mass occupying the right main pulmonary artery with infiltration of mediastinal fat
-
Pulmonary perfusion SPECT-CT: Absence of perfusion in the right lung, indicating complete occlusion of the pulmonary artery
-
Pulmonary function tests: FVC 96%, FEV₁ 99%, DLCO 64%
-
Echocardiography: Normal ventricular function with no pulmonary hypertension
-
These findings confirmed surgical operability, and upfront surgical resection was indicated.
3D Model–Based Surgical Planning
The 3D reconstruction model for this rare case of pulmonary artery sarcoma validated and enhanced the interpretation of conventional CT images. It enabled a clearer mental processing of the tumour’s anatomy and its relationship with the bronchovascular structures, thereby supporting selection of a sternothoracotomy (hemiclamshell) approach over alternative surgical accesses.
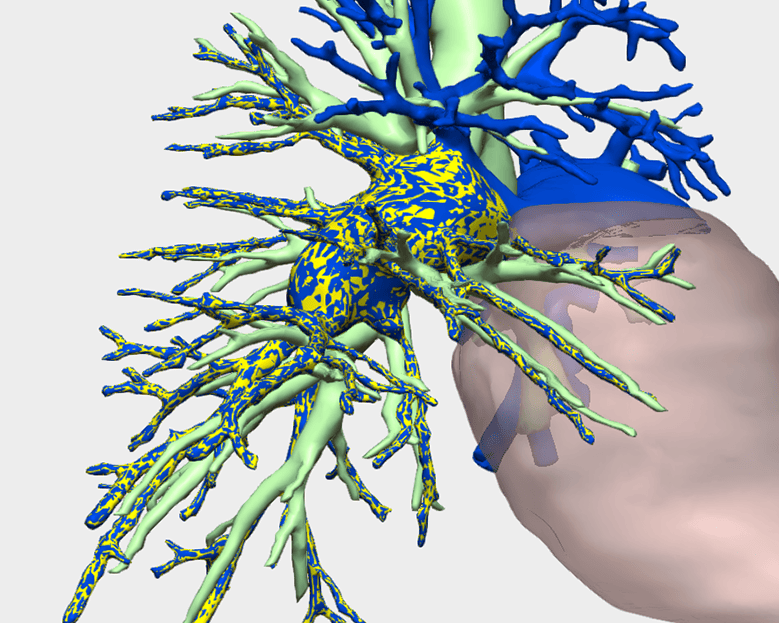
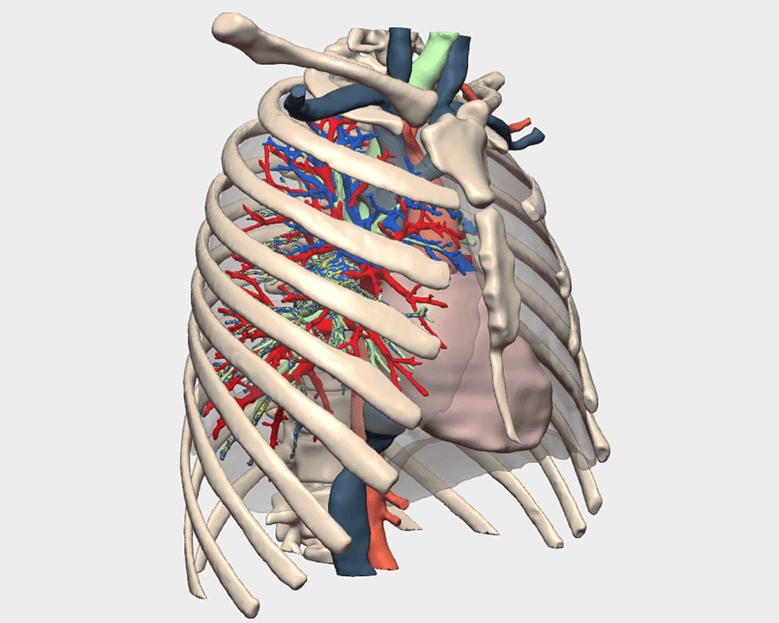
Beyond visualisation, the ability to rotate, manipulate and spatially explore the 3D model allowed the surgical team to mentally rehearse the procedure and anticipate the key steps required for safe dissection and tumour control.
Surgical Approach to Pulmonary Artery Sarcoma
This complex procedure was performed by Dr Carlos Gálvez Muñoz, Consultant Thoracic Surgeon at Hospital General Universitario de Alicante, together with Dr Antonio García Valentín, Consultant Cardiac Surgeon, and Dr Xavier Vaíllo, Thoracic Surgery Resident.
Surgery was carried out via an anterior sternothoracotomy through the fourth intercostal space (hemiclamshell), with preparedness for extracorporeal circulation if required. The main surgical steps included
-
Dissection of the left innominate vein, anterior pericardial opening, and intrapericardial circumferential control of the superior vena cava (SVC) and ascending aorta, with placement of purse-string sutures in the ascending aorta and right atrium in case cannulation became necessary
-
Retraction of the SVC to the right and the ascending aorta to the left, allowing intrapericardial dissection of the right pulmonary artery up to palpation of the proximal tumour margin, located 1.5 cm from the main pulmonary artery
-
Extensive retroaortic mobilisation and circumferential control of the pulmonary artery, followed by vascular stapling and sectioning
-
Dissection, control and sectioning of the intrapericardial superior pulmonary vein
-
Release of dense adhesions between the right lower lobe and the diaphragm, anterior and posterior mediastinum, and chest wall, followed by exposure, dissection and sectioning of the extrapericardial inferior pulmonary vein
-
Connection of intrapericardial and extrapericardial dissections to allow completion of right main bronchus dissection and proximal stapling
-
Systematic lymph node dissection of stations 2R, 4R, 7, 9 and 10, as well as peripheral nodal stations, completing a right pneumonectomy
-
Confirmation of adequate haemostasis and bronchial stump integrity
-
Placement of an anterior bovine pericardial patch to prevent cardiac herniation or laceration, secured with pericardial closure sutures
Surgical Outcom
The patient’s postoperative course was favourable. The chest drain was removed at 48 hours, with stable haemodynamics and no respiratory or other complications. She was discharged on postoperative day five.